Dr. Rice has joined Beacon Orthopedics and Sports Medicine
Congratulations Dr. Rice: 2025 Cincinnati Magazine Top Doctor
Subchondroplasty

A subchondral bone defect, often referred to as a trabecular fracture, marrow edema lesion, or a Bone Marrow Lesion (or BML), is a term for a finding on an MRI that represents an abnormal area or defect inside the bone. BMLs are visible on an MRI but not in a regular X-ray. They are typically found in subchondral bone, the region below the cortical bone near a joint. They can only be seen on certain MRI sequences, such as T2, appearing as a hazy white area against the background of darker bone.
Microscopic analysis has shown that BMLs represent a healing response surrounding small defects in the subchondral bone, such as micro trabecular fractures. In some cases, BML defects are a result of a bone injury that does not heal properly. In other cases, BML may be a stress reaction that forms from overuse or poor joint mechanics.
Conservative treatments for BMLs include pain medications, knee braces, crutches, and physical therapy. However, long lasting (chronic) BMLs that do not heal by themselves will require treatment. Patients with chronic BMLs may have more rapid cartilage loss and may be more likely to require a total knee replacement.
If concservative treatment fails, subchondroplasty is a minimally invasive procedure that is performed to specifically repair chronic BMLs by filling them with a bone substitute material. The bone substitute is then slowly resorbed and replaced with healthy bone repairing the bone defect. Subchondroplasty also resolves the associated edema. Subchondroplasty may be performed alone or along with other arthroscopic procedures.
Ideal Candidate
Patients with a BML may be indicated for subchondroplasty. While indications may vary slightly among surgeons, in Dr. Rice’s practice the best candidates for subchondroplasty present with some or all of the following features:
- Isolated BML (a specific distal femoral condyle, or tibial plateau), rather than global or diffuse marrow edema
- Minimal to mild chondral damage or loss (Outerbridge Grade 2 or less preferred, focal areas of Grade 3 occasionally amenable, Grade 4 typically contraindicated)
- Minimal to no angular deformity (significant varus or valgus alignment of the knee, for instance, predicts poor prognosis with subchondroplasty and is better treated with bracing, osteotomy, joint replacement, or other options)
- Chronic or repetitive microtrauma and subchondral bone stress (these are less likely to heal on their own; acute BMLs equivalent to bone contusions from acute injuries more often heal spontaneously and do not require subchondroplasty)
- Relatively healthy body mass (weight); patients with obesity may be contraindicated
As with most newer technologies and procedures, it is especially important for Dr. Rice to evaluate each patient and case on an individual basis to best determine if subchondroplasty is an appropriate treatment option.
Procedure
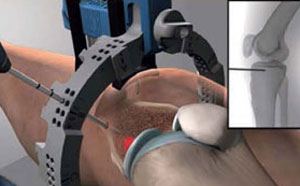
The whole subchondroplasty procedure is performed under fluoroscopy to accurately target the chronic BMLs. Fluoroscopy provides the surgeon with intraoperative real time X-ray images of the surgical area to guide the surgeon. Before the procedure the BMLs are first diagnosed on a T2 Fat Suppressed MRI.
- For subchondroplasty, first, the patient is administered general anesthesia.
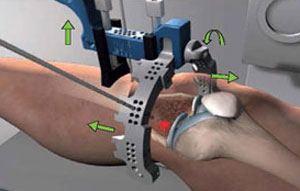
- A semi-circular reference frame is placed relative to the individual patient’s tibia or shin bone. The semi-circular frame allows the surgeon to target the internal subchondral location of BML from a range of trajectories. A pin is inserted through the skin to the bone under fluoroscopic imaging using this semi-circular frame.
- A cannulated drill is then used to advance the pin to the desired depth in the bone.
- The semi-circular guide is then removed leaving only the pin.
- A cannula is placed over the pin and is slid into the bone until it is firmly in place.
- The luer lock of the delivery syringe filled with the bone substitute is attached to the back of the cannula.
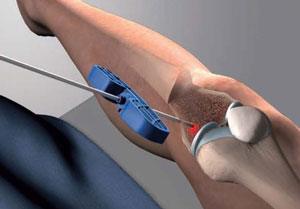
- The bone substitute is then injected into the bone by applying steady pressure. The delivery syringe is then detached. If more bone substitute is required an additional filled syringe may be attached to the same cannula and injected until the desired volume is reached.
- A trocar is inserted into the delivery cannula to push the left behind bone substitute into the bone.
- The cannula is then removed.
- Finally, proper placing of the bone substitute is confirmed using the fluoroscopic imaging and the incision is closed.
Often this procedure is performed in conjunction with joint arthroscopy, when chondroplasty, synovectomy, meniscus repair or resection (knee), and labral repair or resection (hip) may be performed simultaneously.
After the Procedure

Patients are typically treated in an outpatient setting, returning home the same day of the procedure. Some pain and discomfort in the operated area is usually experienced for 1-2 days after the procedure. Pain medications will be prescribed to manage pain. For most patients, the subchondroplasty has no effect on the duration of recovery or restrictions after surgery. Most patients are permitted to bear weight as tolerated after surgery with crutches for support, and participate in physical therapy as part of the routine arthroscopy postop protocol. In the case of knee arthroscopy with concomitant partial menisectomy, recovery is often 4-6 weeks; for meniscal repair, 3-6 months; and hip arthroscopy with labral repair, 4-6 months. These variable recovery periods are dependent not on the subchondroplasty procedure, which is rarely the limiting factor in the surgical recovery, but rather the other procedures performed simultaneously with the subchodroplasty procedure, which may require protection of relatively fragile soft tissue structures.
- For the first 48–72 hours after subchondroplasty procedure, patients will often experience significant pain in the operative area. Rest, ice, compression with ace wrap, and elevation are often helpful during this time. Pain medication is also provided
- Initially walking and standing is performed with crutch support. The use of crutches is typically reduced as tolerated.
- As with virtually every other surgery, proper physical therapy postoperative is critical to success of the surgery and an optimal long-term outcome
Advantages of Subchondroplasty
Subchondroplasty is a minimally invasive procedure with the following advantages:
- It is an outpatient procedure. The patient is usually discharged on the same day as the surgery.
- Compared to more invasive surgeries such as total knee replacement, it may lead to faster recovery and quicker return to normal activities.
- It does not hinder total knee replacement if required in the future.
- It often leads to significant pain relief and restoration of function in patients with symptomatic BMLs
For more information please visit www.subchondroplasty.com/patients.html
nodisplay
nodisplay
Knee Procedures
- ACL Reconstruction
- PCL Reconstruction
- MCL Reconstruction
- LCL Repair And Reconstruction
- Anterolateral Ligament Reconstruction
- All-inside Meniscus Repair
- Menisectomy
- Tibial Tubercle Osteotomy
- Arthroscopic Lateral Release
- Plica Excision
- Loose Body Removal
- Synovectomy
- Infrapatellar Fat Pad Debridement
- Subchondroplasty
- Chondroplasty
- Quadriceps Tendon Repair
- Patellar Tendon Repair
- Total Knee Arthroplasty
- Medial Patellofemoral ligament (MPFL) reconstruction
- Cartilage Procedures: Microfracture, Drilling, Osteochondral Autograft Transfer, Osteochondral Allograft Transplant
- Platelet Rich Plasma


