Dr. Rice has joined Beacon Orthopedics and Sports Medicine
Congratulations Dr. Rice: 2025 Cincinnati Magazine Top Doctor
Meniscus Tear

Meniscus Anatomy and Function
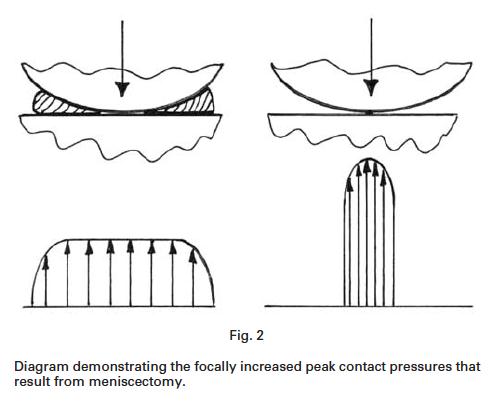
Meniscus refers to two wedge-shape cartilage structures in the knee, also described in shape as C-shaped or semilunar (half-moon), present between the femur and the tibia bones. Medial (inner) and lateral (outer) menisci are present in each knee, in medial and lateral knee joint compartments, respectively. They stabilize the knee joint and act as “shock absorbers,” distributing contact loads more evenly across the entire articular cartilage surface. Loss of the meniscus in a given joint compartment may decrease contact area by 75% and increase contact pressures by 235% as noted in some studies, and therefore loss of the meniscus function has been correlated with rapid and premature onset of osteoarthritis.
Tear Definition, Classification, and Mechanism of Injury
Meniscus tear is a common knee injury in athletes and active people. A sudden bend or twist in may result in meniscus tear, and this is described as a traumatic meniscus tear. Traumatic meniscus tears may occur at any age but represent a higher percentage of tears in younger individuals. In contrast, some meniscus tears occur with no known traumatic injury, and often result from gradual, accumulated microtrauma (‘wear and tear’), compounded by age-related degeneration of the meniscal tissue over time. Older individuals are more prone to these degenerative meniscal tears.
Traumatic versus degenerative tearing provides clues to the prognosis for different types of treatment, the type of treatment recommended, and in the event of surgery, the type of surgery performed.
|
|
Traumatic Tear |
Degenerative Tear |
|
Prognosis with nonsurgical treatment |
Worse if associated with mechanical symptoms such as catching and popping |
Often better amenable to PT, injection, NSAID, activity modification |
|
Type of surgery best indicated |
Arthroscopy with partial menisectomy or meniscal repair (if tear pattern and other factors support repair) |
Arthroscopy with partial menisectomy (repair is rarely possible for these tears); Knee arthroplasty (joint replacement), when degenerative meniscal tearing occurs concomitantly with severe articular cartilage loss |
When diagnosed via MRI, or during surgery, tears can be classified in more specific patterns, such as radial, horizontal, oblique, vertical, bucket-handle, and others. Additionally, tears are often classified by the zone of the meniscus geographically (root, posterior or anterior horn, or mid-body) and biologically (red-red zone in the periphery has the best blood supply and healing capacity, followed by red-white middle zone, and the most inner zone, white-white, which has the worst blood supply and minimal to no healing capacity).
Tear Signs and Symptoms
Torn meniscus symptoms can include pain, swelling, stiffness, catching or locking sensation in your knee. Locking may be so severe the knee feels ‘stuck’ and unable to move through its complete range of motion. For athletes with traumatic meniscus tears, classically swelling and symptoms will arise in a delayed fashion, with most prominent swelling the day after the injury. This is in contrast to knee ACL tears, for instance, in which knee joint swelling is more often immediate. Each injury is unique, and therefore these generalizations will not apply to each patient and each injury.
Diagnosis
Diagnosis includes a combination of history, physical examination, and diagnostic imaging. Physical examination findings suggestive of meniscus tear include joint swelling, tenderness along the joint line, inability to bear weight, and positive findings on meniscus-specific tests such as McMurray’s, Apley’s, and Thessaly’s tests, among others. The sensitivity and specificity of these tests are imperfect, and therefore MRI imaging is generally advised to confirm the diagnosis. Sagittal images are helpful for diagnosing body and posterior/anterior horn tears, while coronal images are helpful for diagnosing root tears and body tears, as well as assessing meniscal extrusion, or displacement from its normal anatomic position.
Treatment – Nonsurgical
The treatment depends on the type, size and location of tear as well as patient age and activity level, with several factors mentioned above. Smaller tears in a more stable pattern, degenerative in nature and without mechanical symptoms and signs, have better success with nonsurgical treatment. This often includes physical therapy, oral or topical anti-inflammatory medication (NSAIDs), and intraarticular cortisone injection. Some studies have demonstrated comparable benefit and success with this treatment compared to surgery for degenerative meniscal tears. However, if the symptoms do not resolve with nonsurgical treatment, surgical treatment may be recommended.
Treatment – Surgical
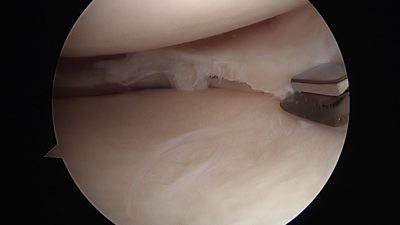
Knee arthroscopy is the commonly recommended surgical procedure for meniscal tears that fail nonsurgical treatment or that have a poor prognosis with nonsurgical treatment. The surgical treatment options include partial meniscus removal (meniscectomy) and meniscus repair. Surgery can be performed using arthroscopy, where a tiny camera will be inserted through a tiny incision, permitting a view inside the knee on a large screen. During meniscectomy, small instruments called shavers or biters may be used to remove the torn meniscus, contouring the remaining meniscus to a smooth, stable rim. In arthroscopic meniscus repair the torn meniscus is sutured to the intact meniscus and joint capsule to structural support the torn fragment and facilitate healing.
For more information about these surgical procedures, please refer to the corresponding pages under the “Procedures” tab.
Case Example #1
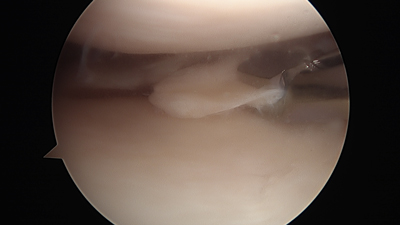
42yo active male cyclist unable to walk or cycle for 4 weeks after sudden twisting injury with swelling and clicking/catching of the knee.
Complex medial meniscus tear of body and posterior horn
Knee Conditions
- Anterior Cruciate Ligament (ACL) Tear
- Posterior Cruciate Ligament (PCL) Tear
- Medial Collateral Ligament (MCL) Tear
- Lateral Collateral Ligament (LCL) Tear (a.k.a. Fibular Collateral Ligament Tear)
- Meniscus Tear
- Chondral defect (a.k.a. osteochondral defect, cartilage injury)
- Chondromalacia Patella
- Patellar Dislocation
- Patellar Instability
- Quadriceps Tendon Rupture
- Patellar Tendon Rupture
- Knee Osteoarthritis
- Bone Contusion


