Dr. Rice has joined Beacon Orthopedics and Sports Medicine
Congratulations Dr. Rice: 2025 Cincinnati Magazine Top Doctor
Anterior Cruciate Ligament (ACL) Tear
One of the most common knee injuries is an anterior cruciate ligament sprain or tear, with an incidence in the United States approaching 200,000 annually. Nearly 150,000 ACL reconstruction surgeries are performed annually in the U.S.
Athletes who participate in high demand cutting sports like soccer, football, and basketball are more likely to injure their anterior cruciate ligaments.
If you have injured your anterior cruciate ligament, you may require surgery to regain full function and stability of your knee. This will depend on several factors, such as the severity of your injury and your activity level. The TriHealth Orthopedic and Sports Institute comprises a comprehensive team of sports medicine orthopedic surgeons, non-surgical physicians, physical therapists, and athletic trainers to diagnose, treat, and prevent ACL injuries.
Injury Description

The classic ACL injury occurs during a non-contact event usually when decelerating, stopping suddenly, twisting, cutting, or jumping. Oftentimes the patient will hear or feel a “pop” at the time of injury and sometimes they may report brief a hyperextension of the knee joint. Immediately after the injury patients may be able to continue activity, however most of the time the patient is unable to continue regular activity and a few hours after injury the knee swells considerably. There is typically tenderness around the joint, loss of full range of motion, and discomfort applying weight to the leg.
When the ACL is injured as a result of direct contact, football is often the associated sport. Most often, the knee is subjected to a direct blow to the lateral side and other ligaments are injured in addition to the ACL. The most common multi-ligament injury is the ‘unhappy triad’ that includes the ACL, medial collateral ligament (MCL), and the medial meniscus.
Several studies have shown that female athletes have a higher incidence of ACL injury than male athletes in certain sports. It has been proposed that this is due to differences in neuromuscular control. Other suggested causes include differences in pelvis and lower extremity (leg) alignment, increased looseness in ligaments, and the effects of estrogen and relaxin on ligament properties.
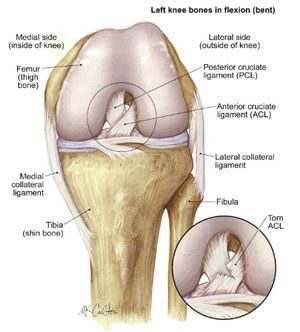
Anatomy
Three bones meet to form your knee joint: your thighbone (femur), shinbone (tibia), and kneecap (patella). Your kneecap sits in front of the joint to provide protection and increase the mechanical efficiency of the extensor mechanism. Bones are connected to other bones by ligaments. There are four primary ligaments in your knee: the ACL, Posterior Cruciate Ligament (PCL), Medial Collateral Ligament (MCL), and Lateral Collateral Ligament (LCL). They act like strong ropes to hold the bones together and keep your knee stable.
Collateral Ligaments
These are found on the sides of your knee. The medial collateral ligament is on the inside and the lateral collateral ligament is on the outside. They control the sideways motion of your knee.
Cruciate Ligaments
These are found inside your knee joint. They cross each other to form an "X" with the anterior cruciate ligament in front and the posterior cruciate ligament in back. The cruciate ligaments control the back and forth motion of your knee. The anterior cruciate ligament runs diagonally in the middle of the knee. It prevents the tibia from sliding out in front of the femur, as well as provides rotational stability to the knee. The ACL sees stress with twisting and pivoting movements.
Injury Grading
About half of all injuries to the anterior cruciate ligament occur along with damage to other structures in the knee, such as articular cartilage, meniscus, or other ligaments. A “bruise” to the bone and cartilage of the femur and tibia occur nearly 100% of the time in acute ACL tears.
Injured ligaments are considered "sprains" and are graded on a severity scale.
- Grade 1 Sprains. The ligament is mildly damaged in a Grade 1 Sprain. It has been slightly stretched, but is still able to help keep the knee joint stable.
- Grade 2 Sprains. A Grade 2 Sprain stretches the ligament to the point where it becomes loose. This is often referred to as a partial tear of the ligament.
- Grade 3 Sprains. This type of sprain is most commonly referred to as a complete tear of the ligament. The ligament has been split into two pieces, and the knee joint is typically unstable.
Partial tears of the anterior cruciate ligament are rare; most ACL injuries are complete or near complete tears (Grade 3).
Physical Examination and Patient History
During your first visit it is important to discuss your overall medical health, activity levels, hobbies and sports participation, and goals for the future, both professionally and in recreation. This will help determine the best treatment for your needs.
During the physical examination, your doctor will check all the structures of your injured knee, and compare them to your non-injured knee. Most ACL injuries can be diagnosed with a thorough physical examination of the knee in a relaxed patient.
Imaging Tests
Imaging tests are used to confirm the clinical diagnosis of an ACL tear:
- X-rays. Although ligaments can not be directly seen on xrays, they can show whether the injury is associated with a broken bone, particularly an avulsion of a small piece of bone that suggests an ACL tear, as in a Segond fracture, a small bony fleck avulsion off the proximal lateral tibia that corresponds with ACL tears. Xrays also reveal overall bony alignment of the knee and lower extremity, permitting the orthopedic surgeon to anticipate any required correction of bony alignment at the time of surgery. Additionally, in young athletes, xrays permit the surgeon to evaluate the growth plates, and select a surgical technique that will be safe for the patient and preserve growth of the long bones to the time of skeletal maturity.
- Magnetic resonance imaging (MRI) scan. MRI creates better images of soft tissues like the anterior cruciate ligament, and is the gold standard non-invasive test for confirming ACL tear. Accuracy of MRI in detecting ACL tears approaches 99%. MRI also permits full evaluation of the cartilage, meniscus, other ligaments, and other soft tissue, and if injury or tears to these other structures are present, they may be addressed simultaneously with ACL reconstruction or in future procedures. For instance, meniscus tears occur commonly with ACL tears, and rates of successful meniscus repair are higher when performed at the same time as ACL reconstruction than when performed alone. The meniscus (50% of multi-structure injuries), medial collateral ligament (30%), or articular cartilage (30%) are the most frequently concurrently injured structures.
Treatment
Treatment for an ACL tear will vary depending upon the patient's individual needs. For example, the young athlete involved in agility sports will most likely require surgery to safely return to sports. The less active, usually older, individual may be able to return to a quieter lifestyle without surgery using physical therapy rehab.
Nonsurgical Treatment
A torn ACL will not heal without surgery. But nonsurgical treatment may be effective for patients who are elderly or have a very low activity level. If the overall stability of the knee is intact, then simple, nonsurgical options may allow a return to activity sooner.
After acute injury, initial steps should be taken to reduce swelling by applying the established RICE principles (Rest, Ice, Compression, and Elevation). Early efforts should be made to regain full ROM, especially extension, and walking with full weight bearing is encouraged 7-10 days after injury. Usually within 1-3 weeks acute swelling has reduced and full ROM is established.
Once full ROM is established, an aggressive rehabilitation program focusing on strengthening and endurance should be followed. The goal of these exercises is to change the quadriceps/hamstring strength ratio from a normal 3:2 ratio to a 1:1 ratio because the hamstring muscles help the ACL prevent forward translation of the tibia on the femur.
When strength is approximately 70% of normal, the rehabilitation program will incorporate a proprioceptive / balancing component using balance boards and other dynamic tools. The goal of this training is to increase stability in the knee joint replicating sport activities.
The last step of the rehabilitation program should assess which activities create pain, discomfort, or instability in the knee joint and actively modify the intensity, duration, or technique of these activities to avoid pain.
Surgical Treatment
Timing
Patients should regain full ROM, reduce swelling, and have quadriceps control prior to surgery. Occasionally patients are involved in a preoperative therapy program and attainment of full ROM can take 2 weeks or longer. It has been speculated that full ROM prior to surgery can decrease postoperative rehabilitation time, and improve postoperative range of motion.
ACL Reconstruction
Surgery for ACL injury is an ACL reconstruction using a tendon graft and is typically performed using arthroscopic methods. The surgeon makes small incisions so that a pencil shaped instrument with a camera and lighting system attached can penetrate inside the knee joint and see the inside structures. The inside of the knee can be seen on a TV screen and the surgeon will perform surgery through several small incision points around the knee.
Graft Options
Graft Harvest Sites
There are three common types of graft harvest sites:
- Patellar Tendon : This commonly includes the central third of the patellar tendon with bone blocks from the patella and tibia; perceived advantages of this graft include high strength, composition similar to the native ACL, and healing of bone to bone, which may be more reliable and robust.
- Hamstring Tendon : Traditionally this includes harvest of the semitendinosis and gracilis tendons, although more recently techniques have been developed using only the semitendinosis in quadrupled form. Hamstring tendons offer ease of harvest and may offer less postoperative pain for the patient in the early recovery period.
- Quadriceps Tendon : Less commonly utilized than the other two grafts but gaining in popularity, quadriceps tendon comprises a thick, strong graft choice that may include a plug of patella bone or be comprised only tendon tissue.
It is important to discuss graft options with your surgeon to select the right graft for you. Some orthopedic research indicates lower re-tear rates with patellar tendon, but a majority of the highest quality research indicates no significant difference among the three graft options, with successful outcomes obtained with all graft choices.
Autograft versus Allograft
In addition to harvest site, another difference in grafts it consider is autograft versus allograft. Allografts are harvested from cadaver donors while autografts are harvested from the patient undergoing ACL reconstruction. Each graft has advantages and disadvantages. Most orthopedic research has demonstrated lower re-tear rates using autograft tissue, and this is generally recommended in young competitive athletes under age 25. However, autograft requires additional incisions and may result in more early postoperative pain. Patients may perceive slower progress decreasing pain and restoring range of motion in the early rehab phase, although autograft completes the ligamentization process more rapidly than allograft tissue. Patients choosing allograft may benefit from less pain immediately after surgery, and may feel better sooner, but the incorporation of the graft into a new ACL may take longer than autograft, and long-term re-tear rates are higher in allograft tissue. Additionally, although increasingly rare given modern testing and sterilization techniques, disease transmission of hepatitis and HIV remains possible, generally considered a 1: 1.6 million risk.
Long Term Expectations
ACL reconstruction surgery has a 90% success rate in terms of knee stability, patient satisfaction, and return to full activity, which comprise the primary goals of surgery. ACL reconstruction should also theoretically protect the menisci from further injury and slow degenerative changes in the knee joint, although orthopedic research proving this effect is still lacking.
The re-rupture rate of a reconstructed ACL is very low, generally 2-5% at an average of 2 years after surgery. Of equal or greater concern is the risk of subsequent ACL injury on the opposite leg, which increases substantially from 1 in 3,000 to 1 in 50.
Patients who opt out of ACL reconstructive surgery may experience further injury to the knee joint, particularly to the menisci. ACL-deficient patents are at higher risk for later meniscectomy, 20% over the 5 years following ACL injury. Also, 70% of ACL deficient patients have signs of osteoarthritis in the knee.
Complications
- Generalized complications such as infection, neurovascular injury, and thromboembolic disease are extremely rare (0.2-0.5%).
- Deep vein thrombosis is another low probability (.1%) complication.
- Graft misplacement complications due to the graft not placed anatomically can lead to motion problems, impingement, and graft failure. Careful attention to detail during surgery must be observed to avoid these complications, and this is increasingly uncommon as surgical techniques and technology have improved
- Other complications include knee stiffness (5-25% incidence), anterior knee pain (10-20%), Patellar tendonitis (20% in 1st year, then rare afterwards), Patella fracture (.3-1.8%).
ACL Injury in Children
Incidence : ACL injuries in patients younger than 14 years vary from 3% to 10%. However, sports are becoming increasingly more competitive at younger ages, thus ACL injury incidence is expected to increase among the younger population.
Treatment : Initially, an ACL injury in children is treated non-operatively, using a similar treatment plan as described above, especially in children with widely open growth centers. With patients who fail conservative, non-operative treatment operative treatment must be considered because recurrent episodes of pivoting cause cartilage and mensical damage, which can lead to early degenerative changes.
Special considerations must be made when deciding whether or not to move forth ACL reconstructive surgery in children. There is possibility of interrupting and/or arresting normal bone growth that can result in significant leg length differences or angular deformity. Physeal-sparing (avoiding growth plate trauma) ACL reconstruction can be performed for younger patients, and improvements and technology and surgical technique have opened this option to many patients previously ineligible for surgery. Nonetheless there remain concerns these surgeries sacrifice accurate restoration of the ACL anatomy for the sake of protecting the growth plates.
New Developments in ACL Reconstruction
While ACL reconstructions have allowed patients to return to high level sports and prevent meniscus tears, the surgery still has room for improvement. Recent studies of patients that had ACL reconstructions 10 years prior still develop early osteoarthritis. There has been a lot of interest in ACL augmentation and double bundle ACL reconstruction. These are surgical techniques that are aimed to preserve or replace the normal ACL in a more anatomic fashion.
ACL Augmentation
With ACL augmentation surgery, the goal is to preserve as much of the original ACL as possible while providing additional support via synthetic high-strength suture material. When the ACL is torn, the two bundles in the ACL may have varying degree of injuries. The attempt is to preserve the patient’s ACL so that it can heal together with the support of suture material, and by definition maintain the original anatomy of the ligament. Concerns with this technique include the poor healing potential of the ACL, although more recent studies suggest it may have better healing capacity than previously believed. Nonetheless this is considered an experimental procedure at this time and may hold promise in the future.
Double Bundle ACL Reconstruction
There are two bundles to the ACL, namely the AM (anteromedial) and PL (posterolateral) bundles. Historically, only one graft is used and the anatomical position of one bundle of the ACL is reconstructed. Two or double bundle ACL reconstructions are performed to reconstruct both bundles of the ACL. This operation technically is more demanding and may be indicated for selected patients such as highly competitive professional athletes. Laboratory testing demonstrates biomechanical superiority of double bundle ACL reconstruction under some conditions, but the benefits have not been clearly observed in real patients undergoing double bundle reconstruction versus single-bundle reconstruction. At this time both surgeries are considered acceptable alternatives and single-bundle reconstruction remains the procedure of choice for the vast majority of surgeries performed in the United States.
Rehabilitation/BOOST Functional Sport Training
Rehabilitation Regardless of surgical or nonsurgical treatment, rehabilitation plays a vital role in getting you back to your daily activities. A physical therapy program will help you regain knee strength and motion. If you have surgery, physical therapy first focuses on returning motion to the joint and surrounding muscles. This is followed by a strengthening phase designed to protect and support the new ligament. The final phase of rehabilitation focuses on a functional return tailored for the athlete's sport. This typically occurs 3-4 months after surgery, and often continues until 9-12 months postoperatively.
Knee Conditions
- Anterior Cruciate Ligament (ACL) Tear
- Posterior Cruciate Ligament (PCL) Tear
- Medial Collateral Ligament (MCL) Tear
- Lateral Collateral Ligament (LCL) Tear (a.k.a. Fibular Collateral Ligament Tear)
- Meniscus Tear
- Chondral defect (a.k.a. osteochondral defect, cartilage injury)
- Chondromalacia Patella
- Patellar Dislocation
- Patellar Instability
- Quadriceps Tendon Rupture
- Patellar Tendon Rupture
- Knee Osteoarthritis
- Bone Contusion


