Dr. Rice has joined Beacon Orthopedics and Sports Medicine
Congratulations Dr. Rice: 2024 Cincinnati Magazine Top Doctor
Femoroplasty (a.k.a. "CAM takedown")

The hip joint is a ball and socket joint, in which the upper rounded end (head) of the femur (thigh bone) articulates with the cavity of the acetabulum in the pelvic bone. The cartilage surface of the femoral head and acetabulum allows smooth movement of the hip joint. Occasionally, the femoral head and/or acetabulum may have an irregular shape due to acquired overuse, or inherent genetic or developmental abnormalities, and is called femoroacetabular impingement (FAI). This can cause damage to the cartilage and tissues that border the articulating surfaces, resulting in pain and limitation of movement. FAI associated with a bump or prominence on the femoral head/neck junction is called Cam impingement. A femoroplasty is a surgical procedure to correct Cam impingement and is indicated when conservative treatments fail to relieve pain.
Femoroplasty is usually performed by a minimally invasive technique called arthroscopy, in which a camera and miniature instruments are inserted into small incisions to reach the hip joint. Bony irregularities on the femoral head and neck are removed and a more anatomic contour is sculpted with a small bone burr. Tissue damage such as labral tearing is typically addressed during the procedure.
After femoroplasty, you may go home the same. You will be advised to use crutches for a period of 4 weeks with 50% weight bearing. Physical therapy is usually recommended immediately following surgery to improve movement and strength, usually within 48-72 hours.
Since the procedure is performed arthroscopically complications are rare but may include nerve injury, femoral neck fracture and heterotopic ossification (bone deposition in soft tissue).
Frequently Asked Questions About Femoroplasty
- How do I decide if I need femoroplasty surgery?
- The need for femoroplasty is often an individualized decision based on complex imaging data from plain x-rays and often MRI and/or CT images. In Dr. Rice’s practice, the most common CAM lesion warranting femoroplasty is focal, in the anterior-superior quadrant, often correlating with the site of labral tearing. This is often best appreciated on “frog” or “Dunn” xray views of the hip, but each CAM lesion is unique and some are better seen on AP or cross-table views, for instance.
- How does a preoperative CT scan help with femoroplasty surgery?
- Preoperative CT scans are routine for Dr. Rice’s patients undergoing hip arthroscopy, as the 3D reconstructed images reveal tremendous detail and help define the exact borders of the CAM lesion, as well as depth. CAM lesions often extend more laterally and inferiorly than are appreciated on hip x-rays alone, and 3D CT scan images help ensure complete resection of the lesion.
- How do you confirm you have resected the entire CAM lesion during femoroplasty surgery?
- Multiple methods are utilized intraoperatively to confirm complete CAM resection. Direct visualization is most often utilized, as an experienced hip arthroscopist develops an understanding of what a properly sculpted hip should look like through the lens of a 70-degree arthroscope. X-ray or fluoroscopic imaging is also utilized during surgery to confirm adequate resection in multiple planes of view, often using AP, frog, cross-table, and other angles to develop a “3D” image in the surgeon’s mind. Emerging proprietary hip arthroscopy software now allows instantaneous intraoperative calculations of standardized measurements such as alpha angle to more objectively quantify improvement from baseline to post-resection. Finally, dynamic assessment involves range of motion of the hip, especially deep flexion, couple with direct arthroscopic visualization to confirm impingement directly observed at the beginning of the surgery no longer occurs after CAM resection. In some ways, the dynamic assessment is most practical, to the degree aggravating positions of impingement can be reproduced in the operating room.
- If I am undergoing hip labral repair surgery, does femoroplasty change my recovery?
- In Dr. Rice’s practice, the addition of femoroplasty to hip labral repair surgery does not significantly change the amount of time on crutches or the overall recovery timeline and return to sport. Regardless, crutches are used 4 weeks with 50% weight-bearing. The rare but serious complication of femoral neck fracture generally occurs early in the postop recovery, and is typically associated with weightbearing noncompliance (patient chooses to bear full weight rather than recommended partial weight during first 4 weeks) or patient experiences a fall or trauma during the early postop period.
Frequently Asked Questions About Acetabuloplasty
Frequently Asked Questions About Femoroacetabular Impingement
Frequently Asked Questions About Hip Labral Repair
Young Athlete with inability to run for 8-9 months
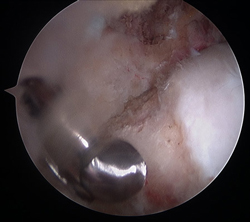
Moderate focal CAM lesion

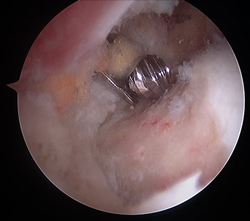
CAM takedown with bone burr
Completed CAM takedown with restored head:neck contour
Hip Scope Labral Repair
nodisplay
nodisplay
Hip Procedures
- Hip Arthroscopy
- Labral Repair
- Acetabuloplasty (a.k.a. "Pincer takedown")
- Microfracture
- Femoroplasty (a.k.a. "CAM takedown")
- Synovectomy
- Ligamentum Teres Tear Debridement
- Iliopsoas Recession
- Subspine Impingement Decompression
- Endoscopic Abductor Tendon Repair
- Endoscopic ITB Release
- Endoscopic Bursectomy
- Proximal Hamstring Repair
- FAI FAQs
- Ischiofemoral Endoscopic Decompression


